Electrosurgery is a cornerstone of contemporary surgical practice, leveraging high-frequency electrical currents to achieve precise tissue cutting, coagulation, and ablation. Two primary modalities—monopolar and bipolar electrosurgery—dominate the field, distinguished by their unique electrical current pathways. These pathways dictate their clinical applications, safety considerations, and effectiveness. This article provides an in-depth comparison, with a particular focus on the high-frequency monopolar electrosurgical unit, a vital tool in minimally invasive procedures, such as those developed by companies like Kangji Medical.
Fundamentals of Electrosurgery
Electrosurgery employs high-frequency alternating current, typically ranging from 200 kHz to 5 MHz, to generate localized heat within tissues. This heat facilitates cutting, coagulation, or desiccation, depending on the waveform and power settings. The high frequency prevents neuromuscular stimulation, ensuring patient safety. While both monopolar and bipolar techniques utilize this principle, their current delivery mechanisms differ significantly.
Principles of Electrical Current in Surgery
In electrosurgery, an electrosurgical unit (ESU) generates a high-frequency current that passes through tissue, where resistance produces heat. Cutting occurs when heat vaporizes tissue, while coagulation results from protein denaturation. The distinction between monopolar and bipolar electrosurgery lies in the path of the electrical current, which influences their suitability for specific procedures.
Historical Context
Electrosurgery dates back to the early 20th century, with pioneers like William Bovie developing early ESUs. Modern high-frequency monopolar electrosurgical units and bipolar devices have evolved to offer enhanced precision and safety, driven by advancements in electronics and surgical techniques.
The high-frequency monopolar electrosurgical unit is a versatile tool widely used in general surgery, gynecology, urology, and thoracic surgery. Its ability to deliver both cutting and coagulation makes it a staple in operating rooms.
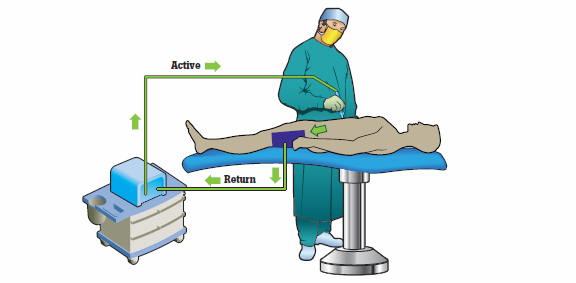
Current Pathway in Monopolar Electrosurgery
In monopolar electrosurgery, the electrical circuit comprises an active electrode (e.g., a blade or probe) and a dispersive electrode (grounding pad). The high-frequency current originates from the monopolar electrosurgical unit, passes through the active electrode into the target tissue, and disperses through the patient’s body to the dispersive electrode, completing the circuit back to the ESU.
The active electrode concentrates the current in a small area, generating intense heat for cutting or coagulation. The dispersive electrode, with its large surface area, ensures the current exits the body with minimal heat, preventing burns. This broad current pathway enables monopolar electrosurgery to affect larger tissue areas, ideal for procedures requiring extensive coagulation or deep tissue penetration.
Clinical Applications
High-frequency monopolar electrosurgical units are employed in:
General Surgery: For procedures like appendectomies or liver resections, where broad coagulation is needed.
Gynecology: In hysterectomies or endometrial ablation, leveraging deep tissue effects.
Urology: For transurethral resection of the prostate (TURP), where precise cutting is critical.
Advantages of Monopolar Electrosurgery
Versatility: High-frequency monopolar electrosurgical units offer multiple modes (cutting, coagulation, blended) for diverse applications.
Broad Tissue Effects: The wide current pathway supports hemostasis over large areas.
Deep Penetration: Effective for procedures requiring deeper tissue interaction.
Safety Considerations
The extensive current pathway poses risks, including:
Burn Risk: Improper dispersive electrode placement can cause burns.
Alternate Site Injuries: Current may flow through unintended paths, especially in patients with metal implants.
Electromagnetic Interference: High-frequency monopolar electrosurgical units may affect pacemakers.
Modern ESUs incorporate safety features like contact quality monitoring to mitigate these risks. Surgeons also use insulated instruments and adhere to strict protocols.
Bipolar Electrosurgery: Current Pathway and Applications
Bipolar electrosurgery excels in procedures requiring precision and minimal current spread, such as neurosurgery or pediatric surgery.
Current Pathway in Bipolar Electrosurgery
In bipolar electrosurgery, the electrical circuit is confined between two closely spaced electrodes, often the tips of a forceps-like instrument. The high-frequency current flows from one electrode, through the tissue grasped between them, to the other electrode, completing the circuit without a dispersive electrode. This localized pathway limits current spread, enhancing safety.
Clinical Applications
Bipolar electrosurgery is used in:
Neurosurgery: For delicate procedures like tumor resection, where precision is paramount.
Ophthalmology: In cataract surgery, minimizing damage to surrounding tissues.
Pediatric Surgery: Where confined current reduces risks in small patients.
Advantages of Bipolar Electrosurgery
Precision: The localized current pathway enables targeted coagulation.
Enhanced Safety: Eliminates dispersive electrode-related risks.
Implant Compatibility: Safer for patients with pacemakers or metal implants.
Limitations
Limited Scope: Effective only for small tissue volumes, less suitable for broad coagulation.
Cutting Constraints: Primarily designed for coagulation, with limited cutting capabilities.
Slower Hemostasis: Coagulation may take longer in larger areas compared to monopolar techniques.
Comparative Analysis of Monopolar and Bipolar Electrosurgery
The choice between monopolar and bipolar electrosurgery hinges on procedural needs, tissue characteristics, and patient safety.
Current Pathway Comparison
Tissue Effects
Monopolar electrosurgery excels in procedures requiring deep or widespread tissue effects, while bipolar is ideal for localized, precise interventions. For example, a high-frequency monopolar electrosurgical unit is preferred for large tumor resections, whereas bipolar is chosen for microsurgery.
Safety Profiles
Bipolar electrosurgery’s confined current pathway minimizes risks associated with dispersive electrodes, making it safer for high-risk patients. Monopolar electrosurgery, while versatile, requires meticulous safety measures.
Technological Advancements
Recent innovations have blurred the lines between monopolar and bipolar applications. Advanced high-frequency monopolar electrosurgical units now offer precision modes, while bipolar devices incorporate cutting capabilities. These advancements enhance flexibility in surgical planning.
Practical Considerations in Surgical Practice
Surgeons must weigh multiple factors when selecting between monopolar and bipolar electrosurgery.
Procedure-Specific Factors
Tissue Type: Dense or vascular tissues may favor monopolar for effective hemostasis.
Anatomical Constraints: Delicate or confined spaces benefit from bipolar precision.
Patient Factors: Patients with implants or comorbidities may require bipolar to minimize risks.
Equipment and Training
High-frequency monopolar electrosurgical units require robust ESUs and trained staff to manage safety protocols. Bipolar systems, while simpler, demand proficiency in handling delicate instruments. Continuous training ensures optimal outcomes.
Cost and Accessibility
Monopolar systems are often more cost-effective for general use, given their versatility. Bipolar systems, while specialized, may incur higher costs for specific instruments. Hospitals balance these factors based on procedural volume and budget.
Future Directions in Electrosurgery
The field of electrosurgery is evolving rapidly, driven by technological advancements and clinical needs.
Innovations in Monopolar Electrosurgery
Next-generation high-frequency monopolar electrosurgical units incorporate AI-driven power modulation, enhancing precision and safety. Features like real-time tissue feedback reduce complications, making monopolar systems more competitive with bipolar in delicate procedures.
Advances in Bipolar Electrosurgery
Bipolar devices are integrating cutting modes and improved ergonomics, expanding their applications. Hybrid systems combining monopolar and bipolar capabilities are also emerging, offering surgeons greater flexibility.
Research and Development
Ongoing research focuses on minimizing thermal spread, improving electrode materials, and enhancing ESU safety features. These efforts aim to bridge the gaps between monopolar and bipolar electrosurgery, optimizing outcomes across specialties.
Conclusion
Monopolar and bipolar electrosurgery represent two distinct approaches to leveraging high-frequency electrical currents in surgery. The high-frequency
monopolar electrosurgical unit, with its broad current pathway, excels in versatile, large-scale applications, while bipolar electrosurgery’s localized pathway ensures precision and safety in delicate procedures. Understanding these differences enables surgeons to select the optimal technique, balancing efficacy, safety, and patient needs. As technology advances, the lines between these modalities continue to blur, promising even greater precision and safety in the future of surgical care.
Comments